The rapid spread of the Mpox virus in just one week across the continent is sending ominous signals about the force of the disease to cripple Africa’s public health. The deadly spread of the infection has triggered frantic decisions by governments and health organizations within and outside Africa. The development has also raised a pertinent question about whether Africa is adequately prepared to fight Mpox to finish? The current Mpox challenge calls for rejigging of the public healthcare services for efficient delivery. It equally provides an opportunity for the continent to mobilize resources to public healthcare development in rural areas, in particular. Gom Mirian analyses that among other issues arising from the Mpox outbreak, the task of enhancing the public healthcare space imposed on the governments contemplates rebuilding the primary health institutions for functional services beyond the level of a consulting clinic.
The Mpox Crisis
The resurgence of mpox (formerly known as monkeypox) has cast a dark shadow over Africa’s health landscape. Once a disease confined to sporadic, localized outbreaks, mpox has evolved into a severe epidemic, causing alarm across the continent. Findings have unveiled their origins, far-reaching effects on communities, and the ongoing response efforts aimed at curbing the crisis.
Mpox Epidemiology
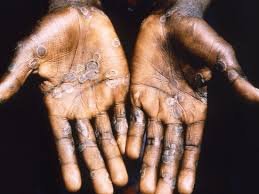
Mpox is a viral zoonotic disease, related to smallpox but generally less severe. It was first identified in laboratory monkeys in 1958 and later found in humans in 1970 in the Democratic Republic of the Congo (DRC). The virus spreads through direct contact with infected animals or humans, presenting symptoms such as fever, rash, and swollen lymph nodes. Historically, outbreaks have been sporadic, but recent years have seen a troubling increase in cases.

According to the World Health Organization (WHO), mpox is transmitted from animals to humans, particularly in areas near tropical rainforests where the virus-carrying animals like squirrels, monkeys, and Gambian pouched rats are prevalent. Human-to-human transmission occurs through contact with body fluids or skin lesions of infected individuals.
A significant concern is the rise in infections among youths under 18 years old. Dr. Kaseya of the Africa CDC reports that about 60% of mpox cases in the DRC are in children under 15, and this figure exceeds 70% when considering those under 18.
Current Situation
As of mid-2024, Africa is grappling with a severe mpox outbreak affecting multiple nations. The DRC remains the epicentre, with thousands of cases reported recently. Nigeria, Central African Republic, and Cameroon are also experiencing rising case numbers. The WHO has noted that cases have more than doubled compared to previous years, with new outbreaks emerging in previously unaffected regions.
Recent data indicates over 17,000 cases continent-wide, with a mortality rate of around 3%. This surge has overwhelmed local healthcare systems, leading to shortages of medical supplies and difficulties in managing patients.
The WHO has declared the ongoing outbreak in Africa a public health emergency of international concern, and the Africa CDC has labelled it a Public Health Emergency of Continental Security. A new clade of the virus began spreading last year, with over 17,000 suspected cases and 517 deaths reported so far in 2024. The number of cases and deaths has significantly increased compared to 2023, with a 160% rise in cases from the previous year.



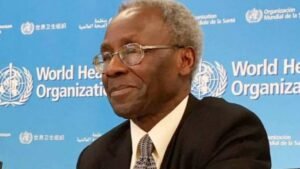
Dr. Jean Kaseya, Director-General of the Africa CDC, stated, “We are seeing an increase in terms of outbreaks in Africa. We are moving from almost two outbreaks per week to three new outbreaks per week.” Currently, 12 countries have reported cases, including DRC, South Africa, Kenya, Rwanda, Uganda, Burundi, CAR, Republic of the Congo, Cameroon, Nigeria, Côte d’Ivoire, and Liberia. Sweden has also reported the first case of the new Clade 1b variant outside Africa.
Dr. Kaseya highlighted the severity, saying, “What is critical to know is that in the past five days, we have had six new countries that are affected.” The DRC continues to account for 96.3% of all cases and 97% of all deaths reported in 2024.
Impact Assessment
The mpox outbreaks have far-reaching effects beyond health, disrupting communities in various ways. In rural areas with limited healthcare infrastructure, the outbreaks have caused severe disruptions. Families face economic hardships due to illness and the loss of income, exacerbating existing health inequalities.
Urban areas have seen increased public health surveillance and pressure on already strained health services. Schools and businesses have faced temporary closures to curb transmission, impacting daily life and economic stability.
Dr. Emmanuel Nguema, a local health official, noted, “Our healthcare systems are under immense pressure. We are doing everything possible, but we need more support, especially in terms of resources and training for our healthcare workers.”
Responses and Interventions
One of the critical interventions needed to control the mpox outbreak is the availability of vaccines. Currently, Africa faces a severe shortage, with only about 200,000 doses available compared to the required 10 million doses, based on vaccination plans from affected countries.
The WHO Regional Director for Africa, Dr. Matshidiso Moeti, stated, “Significant efforts are already underway in close collaboration with communities and governments, with our country teams working on the frontlines to help reinforce measures to curb mpox. With the growing spread of the virus, we’re scaling up further through coordinated international action to support countries to bring the outbreaks to an end.”

In Nigeria, the government has introduced a requirement for travellers to fill out forms at points of entry to monitor and control disease spread. Despite these measures, the Nigerian Centre for Disease Control (NCDC) Director-General Jide Idris reported 39 mpox cases across 33 states and the Federal Capital Territory (FCT) to date.
Expert Opinions
Given Africa’s vaccine shortages, the continent is left relying on alternative preventive measures and interventions. The critical question is are the current responses and interventions adequate to effectively quell the spread of the mpox outbreaks?
In an interview with Africa Health Report, Professor Oyewale Tomori, a renowned virologist and Senior Fellow at the African Centre of Excellence for Genomics of Infectious Disease (ACEGID), emphasised the need for improved surveillance at the Local Government Areas (LGAs) and State levels. “The final remark is a critique of NCDC’s current approach, implying it is ineffective,” Tomori said.
Tomori suggested that the NCDC’s efforts should focus on coordinating rather than controlling surveillance.
He advised on avoiding contact with suspected animals, isolating symptomatic individuals, and ensuring rigorous hand hygiene while highlighting the importance of vaccination.
To him, vaccines like ACAM2000 and Jynneos, are effective against mpox.
Regarding Nigeria’s travel form measure, Tomori noted, “While this is a step toward disease preparedness, it must be handled efficiently”.
“Forms should target high-risk countries to avoid data overload and ensure accurate disease monitoring, he stressed.”
When asked about actions for those exposed to mpox, Tomori advised, “Seek medical attention immediately and adhere to preventive measures like isolation and hand hygiene.”
He also identified key challenges in managing outbreaks, noting, “Repeated failures to learn from past epidemics and inadequate preparedness persist”.
Continuing, he said, “Effective management requires better surveillance, timely detection, and improved health infrastructure”.
Tomori shared insights on the economic impact, stating, “Mpox affects economic activities through lost workdays, isolation, and stigma.”
He called for increased research on virus reservoirs, new treatments, and improved detection methods as crucial for future management.
Future Outlook
The trajectory of the mpox outbreaks in Africa will depend on several factors. Continued international support and resource allocation are vital for managing the crisis. Efforts to improve vaccination coverage and strengthen healthcare infrastructure will be essential in containing the outbreaks.
Research into the virus and its transmission dynamics could offer valuable insights for future prevention and control strategies. Public health education campaigns must address misinformation and promote preventive measures to curb the spread.
Calls to Action/Solutions
The African mpox outbreaks present a formidable challenge, and underscore the need for a robust and coordinated response. While efforts are underway to control the spread and mitigate the impact, the situation remains fluid. Shifting the focus to improve surveillance at local levels and addressing vaccine shortages are critical for managing the crisis effectively.
As Dr. Kaseya warned, “We are losing the youth in Africa.” The priority must be to enhance preventive measures and interventions to safeguard the continent’s future leaders.



