Lassa fever continues to cast a shadow over Nigeria, a viral haemorrhagic disease that remains a persistent public health challenge despite decades of awareness. With 190 deaths recorded in 2024 and 145 deaths reported so far in 2025, the Nigeria Centre for Disease Control and Prevention (NCDC) has documented a relentless burden, prompting urgent scrutiny of why this preventable illness endures. This special report by Sultan Rabiu explores the causes of Lassa fever’s persistence and the barriers to control.
The Scale of the Crisis
Lassa fever, endemic in Nigeria and parts of West Africa, has shown a troubling upward trend in recent years. In 2024, the NCDC reported 1,154 confirmed cases and 190 deaths across the country, reflecting a case fatality rate (CFR) of approximately 16.5%. By early 2025, through Epidemiological Week 1 (30 December 2024 – 5 January 2025), 10 deaths were recorded among 54 confirmed cases, with a CFR of 18.5%, higher than the 11.3% for the same period in 2024.

Cumulatively, 535 confirmed cases and 98 deaths were noted by 11 March 2025, across 14 states, yielding an 18.3% CFR. States such as Ondo, Edo, and Bauchi consistently report the highest caseloads, with Ondo alone accounting for 35% of cases in early 2025. “Lassa fever is not a new disease in Nigeria but, despite continuous control efforts, the 2024 outbreak has not improved notably compared to the previous year,” observed National Lassa Fever Incident Manager, Yetunde Abioye, highlighting the stagnation in progress.
Causes of Persistence
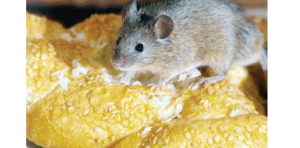
The persistence of Lassa fever stems from its zoonotic nature, transmitted primarily through contact with the multimammate rat (Mastomys natalensis), the natural reservoir of the Lassa virus. Transmission occurs via contaminated food, household items, or direct contact with rodent excreta, with seasonal peaks during the dry season (November to April) due to increased human-rat interaction.


In 2025, data from Epidemiological Week 6 revealed 413 confirmed cases and 80 deaths, with Taraba, Ondo, Bauchi, and Edo states accounting for over 73% of cases, underscoring regional hotspots. Poor sanitation and the cultural practice of consuming rats as a delicacy in some areas exacerbate the risk. Malnutrition and weakened immune systems, prevalent among vulnerable populations, further heighten susceptibility.
Director-General of the NCDC, Dr Jide Idris, noted in December 2024, “While the disease occurs throughout the year, peak transmission typically happens between October and May, coinciding with the dry season when human exposure to rodents increases,” pointing to environmental and behavioural factors as key drivers.
Diagnostic delays also fuel persistence, as Lassa fever’s non-specific symptoms fever, headache, sore throat, and vomiting mimic malaria, delaying testing. The NCDC reported that late presentation significantly increases the CFR, with rates ranging from 1% to 50% depending on healthcare access. Additionally, the 2023 outbreak saw 877 confirmed cases and 152 deaths (CFR 17%) amidst multiple concurrent emergencies COVID-19, diphtheria, and cholera straining resources and complicating response efforts.
Barriers to Control
Several systemic barriers perpetuate Lassa fever’s toll. Inadequate healthcare infrastructure, particularly in rural areas, limits access to timely diagnosis and treatment. Only seven NCDC-coordinated laboratories handle molecular testing, and oxygen therapy critical for severe cases remains scarce in high-burden regions. The 2024 outbreak highlighted poor infection prevention and control (IPC) measures, with 42 healthcare worker infections reported by April 2024 across 11 states.

Community engagement lags, with low awareness and high treatment costs deterring health-seeking behaviour.
The NCDC’s 2024 situational report identified poor environmental sanitation and limited psychosocial support for health workers as gaps, while security challenges in affected regions delay response teams. Médecins Sans Frontières’ expert, Dr Temmy Sunyoto, noted, “What stood out is that we thought we knew everything about how to take care of Lassa fever… but actually we don’t. There are still so many knowledge gaps,” underscoring the need for better diagnostic tools and research.
Solutions and Recommendations
Addressing Lassa fever requires a multi-faceted approach. The NCDC’s activation of Emergency Operations Centres (EOCs) in 2024 and 2025, deploying Rapid Response Teams to states such as Bauchi and Edo, has improved coordination.
Enhanced surveillance, case management, and laboratory capacity supported by seven national labs have increased case detection, as seen in the rise from 25 confirmed cases pre-2018 to 633 in 2018. Public education on hygiene, rodent control (e.g. sealing homes, using traps), and food safety is critical, as recommended by the NCDC’s ongoing risk communication campaigns via radio and social media.
Prevention hinges on strengthening immunisation against co-infections and improving nutrition to bolster immunity.
Treatment with antiviral Ribavirin, when administered early, can reduce mortality, but access must expand. The NCDC’s national action plan, developed with the World Health Organization (WHO), focuses on surveillance, lab capacity, and treatment availability, while the “One Health” approach collaborates with environmental and agricultural sectors to control rodent populations.

Recommendations include governments in high-burden states developing Pneumonia Control Strategies, as suggested by the 2024 joint appeal, and international donors boosting funding for research and vaccine cost reduction via Gavi. Community health workers should be trained to spot cases early, and healthcare facilities must prioritise IPC training to protect staff. Policymakers must address sanitation and security to enable timely responses, ensuring no region is left behind in this fight.
A Call to Action
Lassa fever’s persistence in Nigeria is a preventable tragedy rooted in environmental, systemic, and behavioural challenges. With 335 deaths in 2024–2025 alone, the NCDC’s data demands a robust, coordinated response. As Abioye urged, “There is the need for continued collaboration and community involvement to manage and treat Lassa fever effectively.” By investing in infrastructure, research, and community empowerment, Nigeria can turn the tide against this enduring threat, saving lives and strengthening public health resilience.




Access all betting markets with the secure and official 1win apk.