In this Special Report Juliet Jacob delves into the nation’s public health underbelly to unearth some scandals around the spread of a silent killer called Diphtheria.
A Public Health Scandal in Plain Sight
Despite surging diphtheria infections and fatalities, the Nigerian government’s response has been sluggish at best. Poor vaccine logistics, underfunded health centres, weak community sensitisation, and a crumbling primary healthcare infrastructure have turned diphtheria—a preventable disease—into a deadly epidemic. Experts warn that unless Nigeria urgently develops a clear, coordinated public health strategy, the disease will continue to claim lives—particularly among unvaccinated children and vulnerable populations.
What Is Diphtheria and Why Is It Deadly?
Diphtheria is a bacterial infection caused by Corynebacterium diphtheriae, transmitted through respiratory droplets, coughs, sneezes, or contact with contaminated saliva or mucus. It causes thick grey membranes in the throat that can obstruct breathing, potentially leading to death by suffocation. Left untreated, it may cause paralysis, heart failure, and death.
Dr. Clara Oboh, a Lagos-based infectious disease specialist, describes it as “a killer that takes advantage of system failure,” lamenting that “even though a vaccine has existed for decades, many Nigerians have never heard of it.”
The Numbers Tell a Disturbing Story
According to the Nigeria Centre for Disease Control and Prevention (NCDC), by March 9, 2025, Nigeria had recorded over 25,000 confirmed diphtheria cases and more than 1,300 deaths. The worst-hit states include: Kano – 850 deaths, Katsina – 114 deaths,
Yobe – 109 deaths, Bauchi – 104 deaths, Borno – 68 deaths
Other states affected include Lagos, Edo, Adamawa, and Osun.

Yet, government response has been disturbingly lethargic.
“NO URGENCY”: WHERE IS THE MINISTRY OF HEALTH?
The Federal Ministry of Health has been criticised for its lack of leadership in containing the outbreak. A senior official at a national health NGO, who asked to remain anonymous, said:
“There’s no urgency. There’s no national campaign. We are not seeing coordinated vaccine drives or public education on how to prevent this disease.”
Even in major cities like Lagos, awareness remains abysmal.
“I didn’t even know there was a diphtheria vaccine,” said 32-year-old Segun Alabi, a father of two. “I only read about it online. No health official has ever told us anything.”
A Failure of Public Health Communication
Experts argue that Nigeria’s public health messaging is broken. Unlike during the COVID-19 pandemic, there is no consistent national push to educate citizens about diphtheria.
“Public health is not just about hospitals,” says Dr. Sani Aliyu, former NCDC Director. “It’s about information. If people don’t know there’s a vaccine or what the symptoms are, how can they protect themselves?”

Inside the Outbreak: Interview with Prof. Oyewale Tomori
In an exclusive interview with Africa Health Report (AHR), Professor Oyewale Tomori, virologist and former WHO Regional Virologist, attributed the outbreak to a “backlog of unvaccinated children.”
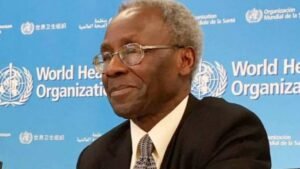
“The outbreak began in May 2022 with isolated cases that were largely unrecorded. Many of today’s victims were never vaccinated in previous years,” he explained.
Citing NCDC data, Prof. Tomori noted:
Between May 2022 and March 2023, Nigeria reported 1,064 suspected diphtheria cases across 21 states.
Of these, 389 were confirmed and only 15.4% were fully vaccinated.
62 deaths were recorded, with a case fatality rate of 15.9%.
Most confirmed cases (78.4%) occurred in children aged 2–14 years.
Prof. Tomori warned that C. diphtheriae is widely present and can infect “the vulnerable and unprotected” through direct contact or airborne transmission.
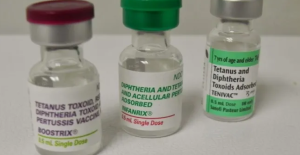
“The best method of prevention is vaccination. DTP vaccines are effective and available, but uptake is poor.”
Age Groups Most at Risk
Children under 15 and adults over 40 are the most vulnerable. According to Tomori:
Fatality rates in children under five range between 5%–10%.
In adults over 40, fatality may reach 20%.
International Perspective: What other Countries Got Right
Countries like the United States, Canada, and Australia have eliminated diphtheria through:
Universal vaccination coverage
Routine surveillance
Strong public education campaigns
These examples highlight what Nigeria could achieve with political will and commitment to public health.
The Role of Primary Healthcare
Nigeria’s primary healthcare system, especially in rural areas, remains underfunded and overstretched. Health centres are often understaffed, poorly equipped, and lack vaccines.
“We cannot vaccinate millions if the last-mile infrastructure is dead,” said Dr. Oboh.
Without strengthening PHCs, there can be no meaningful disease surveillance, early detection, or vaccine distribution.
Prevention is Possible – If Government Acts
Diphtheria is preventable. Health experts recommend: Complete DTP immunisation for children, Wearing face masks in outbreak zones, Avoiding crowded spaces, Early isolation and treatment of suspected cases, Community sensitisation in local languages
World Health Organisation (WHO) Risk Assessment
The WHO notes that diphtheria cases in Nigeria are historically underreported. The last known outbreak before the current wave was in 2011 in Borno State. Current vaccine coverage remains suboptimal, with third-dose coverage of the pentavalent vaccine at only 57% (2021 MICS/NICS survey).
WHO warns that insecurity in parts of the country, especially in the northeast, limits access to healthcare and vaccine distribution. Nigeria is also grappling with other public health emergencies such as Lassa fever, cholera, mpox, and meningitis—further straining limited resources.
Due to a global shortage of diphtheria antitoxin (DAT), timely access to treatment is also under threat.
Recommendations: What Nigeria Must Do Now
Declare diphtheria a national health emergency, Launch a mass awareness campaign across radio, TV, social media, and religious platforms, Fund vaccine procurement and distribution, especially via PHC centres, Train and deploy health workers to rural and underserved areas, Engage traditional and religious leaders for grassroots mobilisation, Publish weekly situation reports and maintain transparent, open data on outbreaks.
Conclusion: Public Health Is a Right, Not a Privilege
Diphtheria should not be killing Nigerians in 2025. With decades-old vaccines available, the continued spread of the disease highlights a dangerous level of governmental neglect. Until Nigeria’s public health authorities prioritise disease prevention and community education, diphtheria will remain a deadly, preventable tragedy—and a damning indictment of state failure.



