[ad_1]
Oguntola Ibukun and Sonia Biose (Lead Writers)
Nigeria, like many other African nations with similar complexities, has had its fair share of challenges in responding to disease outbreaks. In recent years, the country has experienced multiple outbreaks of infectious diseases such as Lassa Fever, Cerebrospinal Meningitis (CSM), Ebola, resurgences of Yellow Fever and Mpox, as well as the COVID-19 pandemic. Nigeria is now facing a deadly Diphtheria outbreak, and as of July 2023, there have been 579 confirmed cases with a case fatality rate of 6.7% among confirmed cases.
Nigeria’s Health Security and the National Action Plan for Health Security
In 2017, Nigeria was classified as “not ready” to handle significant health security threats, achieving a ReadyScore of 39% in the first Joint External Evaluation (JEE) carried out collaboratively by country stakeholders and external evaluators under the guidelines outlined in the International Health Regulations (IHR), 2005.
The JEE, which assesses a country’s capacity to prevent, detect, and respond to public health emergencies across 19 technical areas, identified significant gaps in the country’s public health systems. In the wake of this assessment, Nigeria was presented with an opportunity to improve the country’s ability to prevent, detect, and respond to infectious disease outbreaks.
This led to the development of the National Action Plan on Health Security (NAPHS), a 5-year clear, costed roadmap for implementing the recommendations from the JEE. This multisectoral plan aimed to address the identified gaps highlighted during the evaluation process and was a collaborative effort involving stakeholders from various health-related Ministries, Departments, and Agencies (MDAs), as well as partners from private organisations.
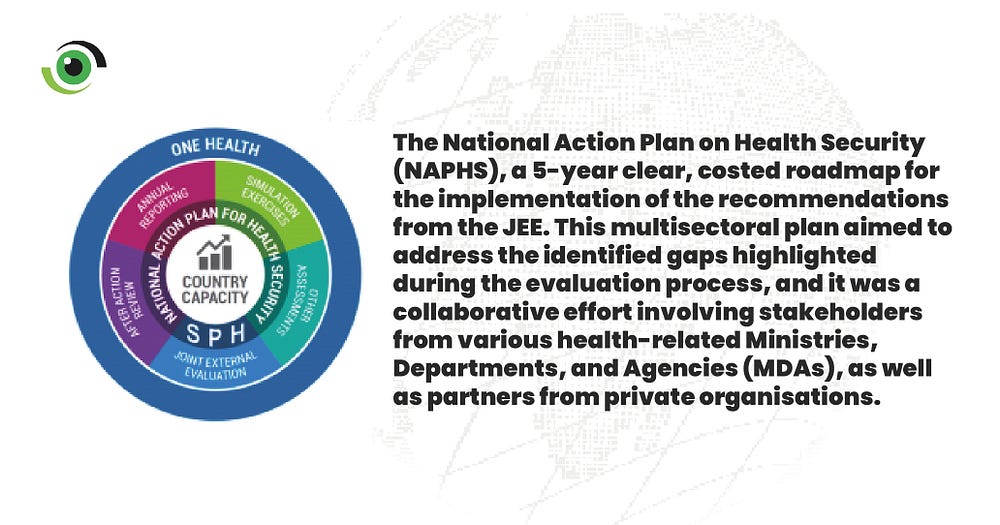
“The country developed the National Action Plan for Health Security looking at the gaps that existed in health security in the country following the JEE and this integrated plans across different MDAs. It was a country-specific activity, costed as a five-year plan,” explained Dr. Oyeladun Okunronmade, Head of Department, Surveillance and Epidemiology, NCDC and Head, IHR unit, NCDC.

Together with the implementation of the NAPHS in 2019, a midterm evaluation was conducted using an updated version of the JEE tool, and it provided an opportunity to measure progress and identify areas for further improvement.
Strengthening Nigeria’s Health Security
Nigeria made substantial strides in bolstering its health security framework following the Joint External Evaluation (JEE) conducted in 2017. This progress can in part be attributed to the implementation of the National Action Plan for Health Security (NAPHS) and the adoption of a one-health approach that fostered collaboration among diverse stakeholders and channeled financial investments into addressing identified gaps.

Transforming Nigeria’s Health Security Infrastructure: Key Milestones and Innovations
The 2023 Joint External Evaluation (JEE) conducted in August 2023 marked a significant improvement in Nigeria’s health security, with a commendable rise in its score from 39% in 2017 to 54% this year.
Among these achievements, one accomplishment stands out as the cornerstone upon which Nigeria’s health security capacity has been fortified: the enactment of the NCDC Act in 2018, giving the IHR focal point the legal mandate it needed to carry out its duties effectively, strengthening the coordination mechanisms and providing a solid foundation for responding to emerging threats, such as the COVID-19 pandemic.

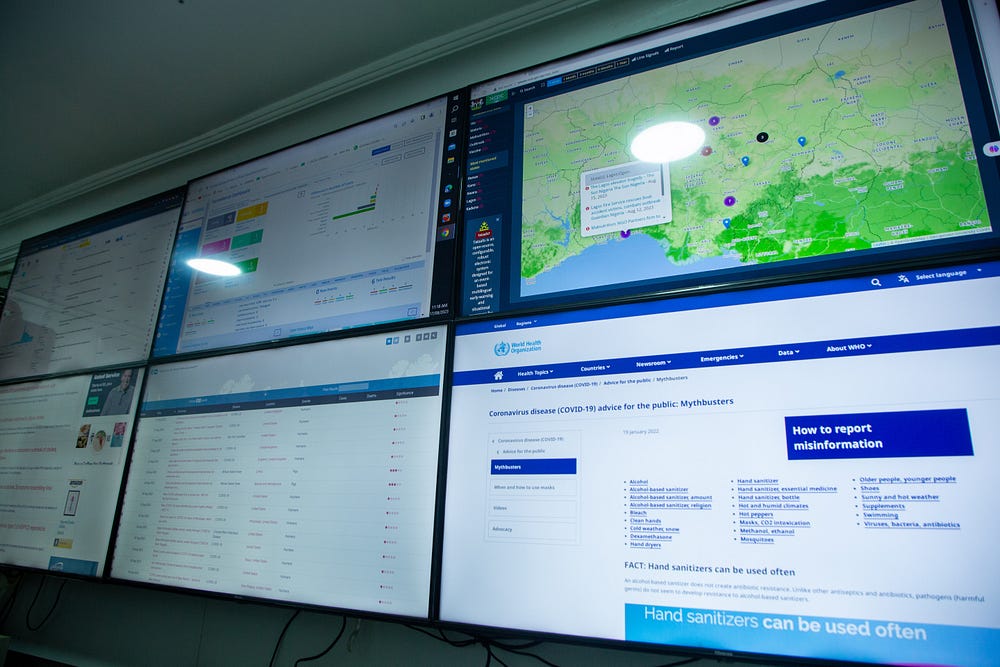
Nigeria’s public health surveillance system has seen significant advancements, notably the state-of-the-art Incident Control Centre (ICC) at the Nigeria Centre for Disease Control and Prevention (NCDC). Collaborating with the Event Based Surveillance Unit (EBSU), they gather and analyse data on disease outbreaks nationwide, using various sources, including online platforms, call centres, and rumour management tools like Tatafo, Epidemic Intelligence from Open Sources (EIOS), Situation Aware (SITAware) and Surveillance Outbreak Response Management & Analysis System (SORMAS), extending their reach to the subnational level for rapid outbreak tracking and response.
Another significant achievement was the establishment of a national reference laboratory (NRL), which houses advanced facilities like the Mega PCR Lab, Multiplex Bead Assay (MBA) Lab, Sequencing Lab, microbiology, serology, and open system PCR lab suite. The NRL also houses the National Biorepository Centre (NBC), accredited by the National Health Research Ethical Committee (NHREC), housing over a million samples from various national surveys for research, quality assurance, and training purposes.
Also worthy of note is the capacity strengthening at points of entry, evidenced by the eight Nigerian ports now included in the WHO’s list of authorised ports for ship inspections and health certificates, strengthening Nigeria’s role in global maritime health security and enabling effective inspections of ships for safety and biosecurity.

Ongoing Challenges and Opportunities for Improvement
Whilst a 15% marked increase in ReadyScore capacity is laudable, this upward trend provides an opportune moment to not only acknowledge the accomplishments, but also to underscore areas that still require persistent attention and development, notably the need for sustained and increased domestic financing for epidemic preparedness-related activities and gender equity in epidemic preparedness and response.
Although substantial progress has been made in enhancing human health security, there remains a pressing need to include and promote the environment and animal sectors within the broader health security framework. The integration of these sectors is crucial for a comprehensive, one-health approach that addresses the interconnectedness of human, animal, and environmental health. Addressing this integration gap will bolster Nigeria’s ability to anticipate and respond effectively to emerging health threats that often originate at the human-animal-environment interface.

Another area requiring focused effort is the capacity at sub-national levels. While notable strides have been taken at the national level, it is imperative to extend these advancements to the subnational regions. Strengthening capacity at this level ensures a more robust and decentralised response mechanism, enabling prompt actions in remote areas. Subnational capacity building entails providing adequate training, resources, and infrastructure to local health authorities, thereby ensuring that Nigeria’s health security improvements are felt throughout the country.
Dr. Henk Jan Ormel, a senior advisor at the World Health Organisation and Lead for the External Evaluation Team, in his closing remarks at the 2023 JEE event said “The country has not yet reached its full potential, and there is much work left to do. He emphasised the need to address identified gaps, draw valuable lessons from the COVID-19 pandemic and other health emergencies, and integrate these insights into the next phase of NAPHS implementation.

“We need to prioritise health,” said Dr. Ifedayo Adetifa, the Director General of the NCDC, adding that healthcare extended far beyond the construction of physical infrastructure. “You need the human capital, equipment, training, and quality systems. Equally, once we get the political leadership to properly prioritise health, then health will receive more funding,” he noted.
In the Coordinating Minister of Health and Social Welfare’s four-point agenda for the health sector, following the just concluded three-day ministerial briefing, the Honourable Minister highlighted improving health security as a key priority. This JEE could not have come at a better time. With a new administration in office, it provides a remarkable opportunity to advocate for enhanced investment to strengthen health security in Nigeria.
[ad_2]
Source link



