[ad_1]
By Hadiza Mohammed and Misbahu El-Hamza (Lead Writers)
The Boko Haram insurgency has had a significant and far-reaching impact on healthcare in northeastern states like Yobe, Borno, and Adamawa. The insurgency disrupted health service delivery, particularly for pregnant women, newborns, and children. For example, in Damaturu Local Government Area (LGA) in Yobe State, although there was an increase in antenatal care (ANC) visits between 2013 and 2014, only 33% of pregnant women received ANC from skilled providers in the state in 2013. This number dropped to 19%, according to the Nigeria Demographic Health Survey 2018 (NDHS 2018).
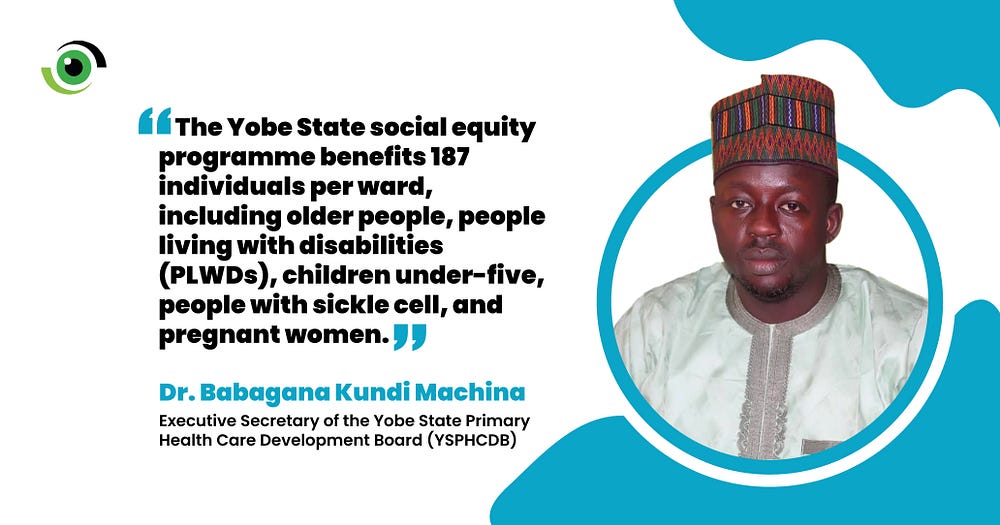
To bridge the healthcare delivery gap, in 2020, the Yobe State Government and its partners collaborated with Plan International, German Cooperation (GIZ), the World Bank’s Saving One Million Lives Project, and other partners to construct, refurbish, and equip PHCs in the state. Dr Babagana Kundi Machina, Executive Secretary of the Yobe State Primary Health Care Development Board (YSPHCDB), said the objective was to establish at least one PHC in the one hundred and seventy-eight wards by 2023 to increase access to essential services.
According to Dr Muhammad Lawan Gana, the State Commissioner for Health, 138 PHCs have either been built, upgraded or rehabilitated as of May 2023. However, they were only able to achieve 78% of the target due to funding challenges. “We realised that the initial bill of quantities and contract sum were insufficient,” he said. So far, four general hospitals have been upgraded to specialist facilities, and eight PHCs to general hospitals.
Building resilient health infrastructure
Gwange Primary Health Centre (PHC) in Njiwaju Gwange Ward, Damaturu LGA was rehabilitated and commissioned in December 2022. The facility now has separate male and female wards, a laboratory, spacious antenatal care (ANC) and immunisation rooms, and additional staff quarters. It offers maternity care services to pregnant and breastfeeding women, including antenatal and postnatal care and delivery and child health services like immunisation. It also provides 24-hour services for women in labour and out-patient care.

After its renovation, the Gwange PHC is now bustling with activity, and among those benefiting from the improved facility are expectant mothers receiving ANC. Photo credit: Nigeria Health Watch
Esther Salihu, officer-in-charge (OIC) of Gwange PHC, said that before the renovation, the facility could accommodate 20 to 30 pregnant women monthly for ANC and a little less than 20 deliveries due to limited space and resources. Currently, about 100 women access ANC services on each ANC day and deliveries have risen to 60–70 monthly. Amina Sherrif, the family planning focal person at the PHC, also reported an increase in women accessing family planning services from less than 100 to about 300 monthly. Fannah Mohammed, a 32-year-old mother of ten, has visited Gwange PHC for 13 years. Reacting to its transformation, she said, “In the past, we only came here for immunisation, but now the hospital has grown big”.
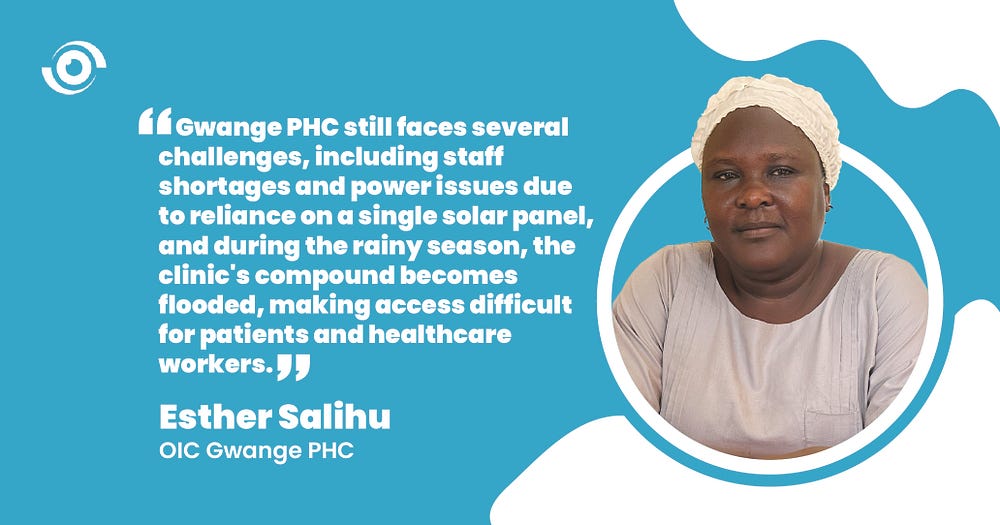
Image credit: Nigeria Health Watch
However, Salihu revealed that the PHC is grappling with multiple issues, including a shortage of staff and power challenges due to reliance on a single solar panel for electricity. Moreover, during the rainy season, the clinic’s compound becomes flooded with water, posing significant challenges for patients and healthcare workers attempting to access the facility.
Expanding social equity
Beyond just rehabilitating and upgrading the health facilities to ensure that the residents of the state use the facilities, in June 2022, the State Government launched a programme called the ‘Buni Expanded Free Healthcare Scheme’ — a fully funded social equity programme to cover basic healthcare needs. Beneficiaries include older people, people living with disabilities (PLWDs), children under-five, people with sickle cell, and pregnant women. The state has 187 wards, and at least 187 beneficiaries are selected from each ward — prioritising 100 pregnant women — to participate in the programme. Once a woman gives birth, she exits the programme, making space for others. Children under five, older people, and PLWDs participate for two years without enrolment. However, people with sickle cell are allowed to renew enrolment due to their specific medical condition. The programme currently has about 42,000 participants.
Mohammed, also a programme beneficiary, said that services are not entirely free as pregnant women must pay an “affordable amount” during delivery. The OIC explained that the affordable amount was only 10% of medication costs, saying the programme covers all other expenses.
In January 2023, the Yobe State Primary Health Care Development Board (YSPHCDB) partnered with the Bill & Melinda Gates Foundation to enrol an additional 2,500 beneficiaries into the scheme in 10 health facilities across 10 LGAs. The intervention is projected to span three years.

Bulama Lawan Kurma, chairman Njiwaju Gwange ward development committee (WDC), voluntarily ensures immunisation adherence, organises monthly meetings with health workers, and skillfully monitors defaulters using registers to maintain up-to-date vaccinations for all. Photo credit: Nigeria Health Watch
There is also the Basic Health Care Provision Fund (BHCPF), a federal government-funded scheme which provides free minimum basic healthcare to the poorest and most vulnerable Nigerians through accredited PHCs to reduce maternal, newborn, and under-5 deaths. Thirty-two thousand beneficiaries across the 17 LGAs in the state are registered in the scheme. “The two financial interventions in the state were designed to be mutually exclusive such that no beneficiary is duplicated simultaneously,” said Dr Machina. However, several communities are not benefiting from either of the social equity programmes.
Fostering progress
According to Shettima Mukhtar, the Director of Planning Research, Monitoring, and Evaluation at the YSPHCDB, the 2021 Multiple Indicator Cluster Survey (MICS) revealed an increase in immunisation coverage within the state. Between 2017 and 2021, the percentage of fully immunised children rose from six per cent to 49%. Furthermore, the first and last ANC visits experienced growth, with a 1.7% and 49% increase, respectively. The report also showed a 77% improvement in family planning service uptake between 2017 and 2021. Additionally, the state’s coverage of the Penta3 vaccine for 14-week-old babies rose from 9% in 2015 to 65% in 2021, earning Yobe State recognition as the “most improved state in immunisation by the NPHCDA,” said Dr Gana.
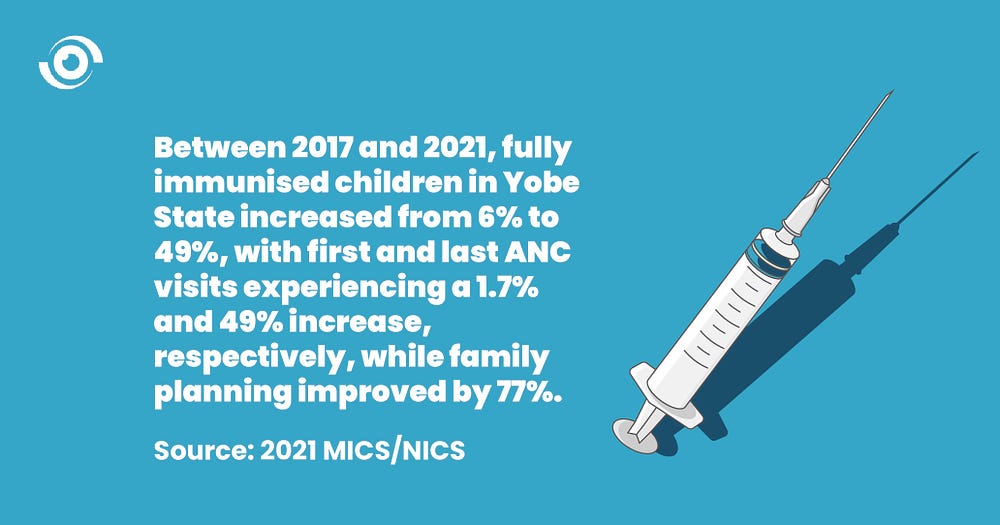
Image credit: Nigeria Health Watch
Though challenges persist, such as the need to address staff shortages and ensure equitable access to social equity programmes for all communities in the state, Yobe State’s commitment to expanding healthcare access and providing free basic healthcare to vulnerable populations demonstrates a dedicated approach to improving the well-being of its people. However, the true measure of success for interventions like these will be evident when reduced maternal and neonatal mortality rates are reported, along with improvements in other health indicators in the state.
.
It is, therefore, critical to ensure the sustainability and long-term effectiveness of these interventions. This can be achieved through fostering collaborative partnerships, implementing continuous monitoring and evaluation mechanisms, and making strategic resource allocations to strengthen the healthcare infrastructure and overcome current challenges.
[ad_2]
Source link



