[ad_1]
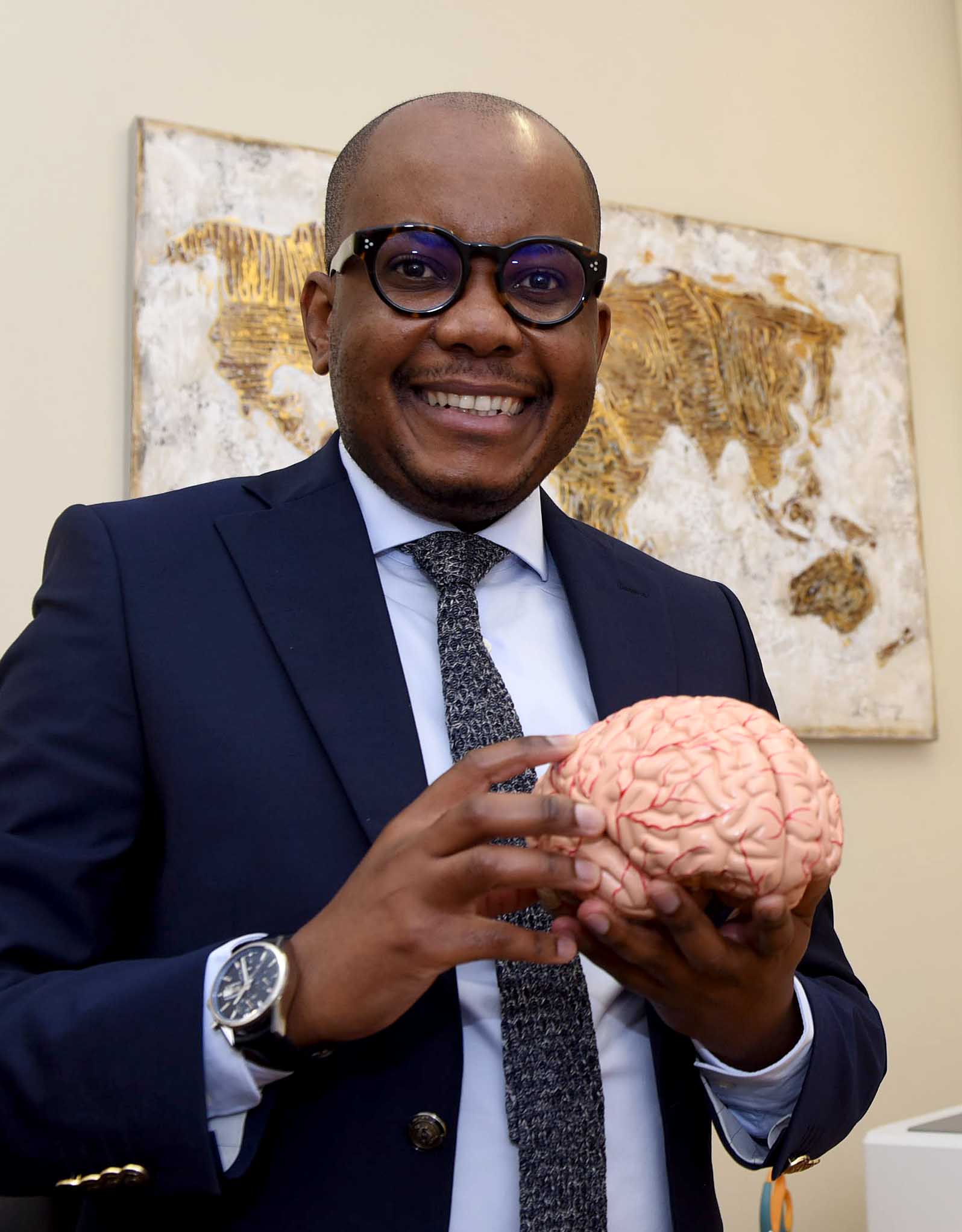
 Dr Lebogang Phahladira earlier this month received a major global schizophrenia research award. PHOTO: Nasief Manie/Spotlight
Dr Lebogang Phahladira earlier this month received a major global schizophrenia research award. PHOTO: Nasief Manie/SpotlightNews & Features
29th May 2023 | Biénne Huisman
In his Twitter biography, 40–year–old Dr Lebogang Phahladira describes himself as “a rookie clinician-researcher who keeps trying and trying”. Now, he is just back from Toronto, Canada, where he received a major global schizophrenia research award.
Jetlagged from his long flight, Phahladira is speaking to Spotlight via Zoom from a rural home near Bela-Bela in Limpopo – where he is visiting family – before he returns to Cape Town.
In Toronto, he received the Global Schizophrenia Award, conferred by the Schizophrenia International Research Society (SIRS). He was a joint winner alongside Professor Natália Bezerra Mota, a computational psychiatrist at the Federal University of Rio de Janeiro, in Brazil.
Related Posts
Commenting on the award, Phahladira says, “It’s easy to do research in developed countries, but in Africa, we work in resource-constrained settings with competing priorities, where mental health is low down on the list in terms of funding and other opportunities. To be recognised by peers on an international front is very humbling.”

Dreams by candlelight
Phahladira was raised by his maternal grandparents and grew up in a remote part of Limpopo near Modimolle (Nylstroom), where they did not have electricity. He recalls studying for his matric exams by candlelight. At the time, his parents were based in Johannesburg and wanted to shield their son from unrest in the city’s townships.
In 1999, aged 16, Phahladira matriculated at Meetsetshehla Secondary School, which was built by a local farmer.
From early on, Phahladira wanted to become a doctor and worked hard to excel at school. He was accepted to study at then MEDUNSA (Medical University of Southern Africa) thirty kilometres outside of Pretoria.
He recalls the shock of moving to a big city. “In the beginning, it was hard, not so much academically, but socially. You can imagine coming from a small town where you didn’t have electricity or running water, where you walked to school come rain or sunshine. Now you’re in this big city all on your own. But it got better in the second year. I had a good experience of university overall.”

Cause and effect in psychiatry
While completing his Bachelor of Medicine and Bachelor of Surgery degree at MEDUNSA, his specialisation interest switched from gynaecology to psychiatry. He explains that in most scientific fields, including medicine, cause and effect are quite linear. Whereas psychiatry was different, which intrigued him.
“In medicine, blood results or an X-ray would tell you that a condition could be TB, or whatever. But in psychiatry, every patient is different. Every patient’s symptomatology is different – the way the disease presents is different. And patients with the same disease respond to different kinds of medication. And this makes it very fascinating. Mental health and the brain and the mind are fascinating. There is a lot we don’t know, so it is an important area for continuous research – trying to solve some of the mysteries of mental illness.”
‘a fascinating illness’
In 2012, Phahladira completed postgraduate training in psychiatry at the University of Cape Town (UCT), after which he joined Stellenbosch University (SU) as a senior lecturer. Here he is a member of the Psychosis Research Programme headed by Professor Robin Emsley. Phahladira obtained his PhD last year, which focused on long-term outcomes in schizophrenia.
“We examined the factors that influence the long-term trajectory of the illness. The understanding is that if we treat patients very early at the onset of illness, at the break of symptoms of psychosis, there is a narrow window of opportunity where we can prevent the poorer outcomes,” he says.

Phahladira adds that his initial research interest had been pathological gambling, but that he decided to focus on schizophrenia due to expertise on the disease at SU. One of the research unit’s ground-breaking initiatives is using long-acting injectables to treat psychotic patients.
Speaking rapidly and with obvious enthusiasm, Phahladira again uses the word “fascinating” to describe schizophrenia. “It is the only illness of humankind that affects everything that defines who we are as human beings. It affects what we think, it affects what we believe, it affects what we perceive, what we hear. Sometimes what we feel, it affects what we remember. And that was one of the attractions for me – to try and dig a little bit deeper and contribute some new knowledge on this fascinating illness.”
Discussing factors that could trigger the onset of schizophrenia, he says, “There are people who hold a strong view that maybe schizophrenia is a neuro-developmental disorder. So the full expression of the disease in late adolescence to early adulthood may stem from as far back as pregnancy – the nutritional status of your mother, the mode of delivery, childhood trauma, abuse, or neglect. It’s still a mystery, but in most cases there might be precipitating factors like stress, use of cannabis, migration is an increased risk, for example, moving to a dense urban centre.”

In April last year, Phahladira tweeted a photograph of his doctoral graduation day, captioned “The joy in my heart! #SUgrad”. Dressed in a scarlet robe and clutching his degree, joy is written on his face. The tweet went viral, eliciting widespread congratulations.
Be wary of ‘putting patients in boxes’
In Cape Town, Phahladira lives in Brackenfell. He has co-authored thirty-five peer-reviewed journal articles and spends most of his working time at the Lentegeur Hospital in Mitchells Plain, a mental health facility affiliated to Stellenbosch University, where he heads the adult psychotherapeutic unit.
“We’ve got people with all kinds of personality disorders – borderline personality disorder, narcissistic personality disorder, bipolar, and so on but sometimes even just voluntary patients with depression or anxiety disorders,” he says.
In the field of psychiatry, diagnostic tools remain controversial and, according to Phahladira, have “significant limitations”. He explains that classifying mental health disorders is often not clear-cut and that each patient’s unique presentation influences diagnosis, choice of treatment, and prognosis.
“So those classifications, they’re helpful to some degree, but the problem with a lot of mental disorders is that they’re not categorical. There is a high degree of shared symptomatology. For example, a person with schizophrenia may hear voices and those kinds of experiences might be present in another patient with bipolar disorder.”

He says mental healthcare workers should be wary of “putting patients in boxes” or sharing a diagnosis with them. “I always say to my patients that the diagnosis does not matter. What matters is how we understand your symptoms. To what extent do they cause impairment in your life and what possible treatment interventions can we offer you? So the labels are less important than the individual experiences of the patients. And I think many of us forget that.” He adds that in some circumstances, particularly in the private sector, such “labelling” is done to unlock medical scheme benefits that cover medications.
Career fulfilment
Responding to if he can recall a moment of career fulfilment for him, he says, “In psychiatry, fulfilment is when you see a patient who has been very ill, where they have lost hope, the family has lost hope, and then they get better,” says Phahladira. “There was a young man, a local Capetonian, his first episode of psychosis happened when he was a first-year law student. Towards the end of his first year, there was an insidious onset of symptoms and it was very, very difficult for the patient and for the family. He started hearing voices, was paranoid, had persecutory ideas, started acting strangely, social withdrawal, not engaging with family, not bathing, you know, deterioration in self–care. Within a few weeks, he became very, very ill to the extent that he could not continue with his studies.”

Phahladira says it was not clear why the man suddenly presented with schizophrenia. “There was no cannabis, there was no family history, there was no trauma. We treated it aggressively with anti-psychotic medication – supported the family, supported the patient. He was in hospital for just over three months. Usually, it takes about four to six weeks to get patients to settle on medication, but he needed more time.
“But now he’s better and he should be graduating towards the end of this year. And I hope that we will be able to support him for as long as we need to. And this is fulfilling, if he is able to achieve his full potential, graduating, and becoming a legal practitioner in the country.”
The World Health Organization (WHO) estimates that schizophrenia affects approximately 24 million people or 1 in 300 people worldwide. In South Africa, reliable prevalence data appears to be lacking, but existing research suggests that around 1% of people in South Africa might be living with schizophrenia. “The prevalence of schizophrenia and other psychotic disorders varies between countries and rural and urban areas,” says Phahladira. “The increased number of people accessing mental health services may be explained by the increase in population, migration, substance abuse, and other environmental factors such as trauma and violence.”
He points out the inextricable link between poverty and unfavourable mental illness recovery. Simply put, without money, early detection and the prolonged treatment and medication required to get better is often inaccessible.
Phahladira speaks passionately about the mental health impacts of climate change on vulnerable people. “I think climate change on the African continent is going to have dire consequences for the most vulnerable. In anticipation of probably the greatest human tragedy, we need to start talking about how climate change will affect health services and presentation of mental health disorders, treatment response, and pathways to care. We need to make sure that we are prepared… and that when the consequences of global warming are at our doorstep, the most vulnerable people and health services are protected.”
*For more information on schizophrenia, the South African Depression and Anxiety Group offers this pamphlet.
[ad_2]
Source link