[ad_1]
Sodiq Ojuroungbe
The World Health Organisation has announced the expansion of the scope of the WHO Director-General’s flagship initiative on tuberculosis over the period from 2023 to 2027 to support fast-tracking progress toward ending TB and achieving universal health coverage by 2030.
The global health agency also called for improved access to tuberculosis prevention and treatment globally.
WHO stated this in a statement issued in commemoration of the 2023 World Tuberculosis day, noting that the global health agency is committed to supporting countries to step up their response to TB control through the expansion of access to services to prevent, detect and treat TB.
The global health organisation stressed that the expansion was part of its journey towards universal health coverage, and to strengthen defences against epidemics and pandemics.
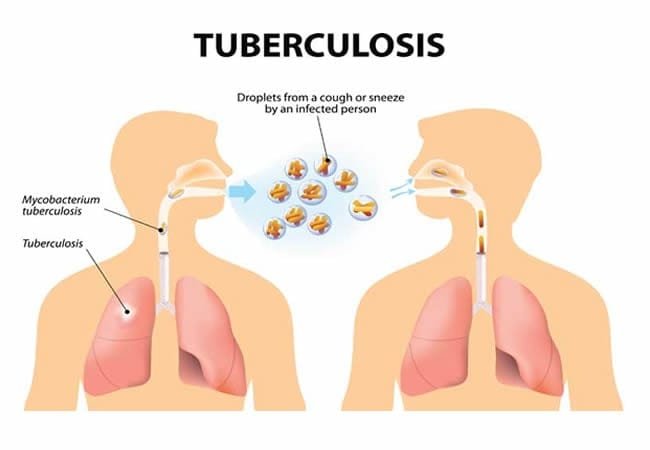
While noting that tuberculosis remains one of the world’s top infectious killers, WHO lamented the increase in the number of people falling ill with TB and drug-resistant TB, alongside an increase in deaths, adding that it was the first time in two decades that was happening.
The WHO Director-General, Dr. Tedros Adhanom Ghebreyesus, noted that the COVID-19 pandemic coupled with ongoing crises such as armed conflict, food insecurity, climate change, and political and economic instability, has reversed years of progress made in the fight against TB.
He said, “TB is preventable, treatable, and curable, and yet this ancient scourge that has afflicted humanity for millennia continues to cause suffering and death for millions every year.
“WHO is committed to supporting countries to step up their response, by expanding access to services to prevent, detect and treat TB as part of their journey towards universal health coverage, and to strengthen their defences against epidemics and pandemics.
“The WHO DG flagship initiative on TB builds on the progress achieved and lessons learned from 2018-2022. It aims to scale up the delivery of quality care to people living with TB through equitable access to WHO-recommended rapid diagnostics, shorter all-oral treatment for infection and disease, increasing their access to social protection and other innovations including digital tools for health.
“The initiative highlights the pressing need to increase both domestic and international investments in TB services, research, and innovation, particularly in new vaccine development. It calls for TB services and programmes, particularly in countries with a high TB burden, to be recognized as an essential component of health systems, bolstering primary healthcare and pandemic preparedness and response.”
Dr. Ghebreyesus further explained that the DG’s flagship initiative is aimed at driving multisectoral action in tackling key drivers of the TB epidemic.
He listed the key drivers as poverty, undernourishment, diabetes, HIV, tobacco and alcohol use, and poor living and working conditions, among others.
He added, “World Tuberculosis Day this year is being commemorated under the theme ‘Yes! We can end TB!’ with the goal of promoting optimism and fostering high-level leadership, increased investments, rapid adoption of new WHO recommendations, and strengthened multisectoral partnerships to combat the TB epidemic.
“As part of the DG Flagship initiative, a special call to action is being issued by WHO and partners urging Member States to accelerate the rollout of new WHO-recommended shorter all-oral treatment regimens for drug-resistant TB.
“Drug-resistant TB continues to be a pressing public health concern, taking a significant toll on individuals affected by TB, communities, and healthcare systems worldwide. In 2021, nearly half a million people fell ill with multidrug- or rifampicin-resistant TB (MDR/RR-TB), and only one in three accessed treatment.
“New WHO guidelines on drug-resistant TB treatment recommend rapid roll-out of the novel BPaLM/BPaL regimen that has the potential to significantly increase cure rates due to its high effectiveness, offer more extensive access because of its lower cost, and improve patients’ quality of life, as it is an all-oral treatment that is considerably shorter than traditional regimens.”
Copyright PUNCH
All rights reserved. This material, and other digital content on this website, may not be reproduced, published, broadcast, rewritten or redistributed in whole or in part without prior express written permission from PUNCH.
Contact: [email protected]
[ad_2]
Source link